 Boy or girl? 'Predict' your baby's gender with this Chinese pregnancy calendar, Lifestyle News - AsiaOne
Boy or girl? 'Predict' your baby's gender with this Chinese pregnancy calendar, Lifestyle News - AsiaOneWarning: The NCBI website requires JavaScript to operate. Ministry of Health, Ministry of Health, Ministry of Health, Ministry of Health and Health MethodsThe standard fetal biometry and soft tissue parameters were prospectively evaluated in third-quarter pregnancies using three-dimensional ultrasound. Growth parameters included the biparietal diameter (BIPARIETAL DIAMETER (BPD), the head circumference (HC), the abdominal circumference (AC), the mean circumference and the length of the femoral diaphysics (FDL). The parameters of the soft tissue included the volume of the fractional arm (AVol) and the volume of the fractional thigh (TVol) that were derived from 50% of the lengths of the humeral or femoral diaphysics, respectively. The percentage of neonatal body fat (%BF) was determined within 48 h of delivery by means of a pediatric air displacement sensing system based on principles of densitometry of the entire body. Linear and cross-sectional regression analysis was performed with possible prenatal predictors and %BF as a result variable. ResultsOcho and seven newborns were studies with an average ± SD %BF of 10.6 ± 4.6%. TVol had the highest correlation with the newborn %BF of all single parameter models. This parameter explained 46.1% of variability in %BF and the best linear regression model is as follows: %BF = 0.129 (TVol) – 1.03933 (PConclusions During the third trimester of pregnancy %BF is very correlated with TVol. Similar to the actual weight of the birth, this soft tissue parameter represents a significant improvement in the explanation of the variation of the neonatal %BF compared to fetal AC or EFW alone. INTRODUCTION Fetal growth is the result of complex interactions between several maternal-fetal and placentero mechanisms. A final classification of the results of neonatal growth depends on how this development is defined. Most obstetricians depend on the height of the uterine fund, the fetal abdominal circumference (AC) measurement and/or a sonographic estimate of the fetal weight for the detection of intrauterine growth restriction (IUGR). More than four decades ago, Battaglia and Lubchenco developed a historical classification of the results of neonatal growth and this statistical approach has also been applied to the evaluation of the fetal weight. The fetal size is generally categorized on the estimated fetal weight (EFW) basis being small (thoth percentile, LGA) for gestational age. Unfortunately, this approach does not distinguish between small or large fetuses, but otherwise normal, from others that are truly malnourished. The evaluation of soft tissue can provide additional information on the generalized fetal nutritional status. Several related parameters have been used, such as the average fat of the arm and the lean mass, the high mean fat and the lean mass, the abdominal fat mass, the subscapulular fat mass, the cheek diameter to the cheek and the buttocks to evaluate the composition of the fetal body. We previously reported that the volume of the fractional extremity can be used for the evaluation of fetal growth and the estimation of the weight using three-dimensional ultrasonography (3DUS). These measurements are reproducible and are obtained quickly because only five cross-cutting slices need to be tracked around half. In addition, this technique is more likely to allow clear visualization of the borders of soft tissue and a safer tracing around each volume slice because only the average part is analyzed. After birth, the neonatal composition of the child's body is traditionally evaluated using the weight of the birth and anthropometric measurements, including the weight and thickness of the skin fold., Hydrostatic weighing is not suitable for studies of newborn body composition because full water submersion is necessary to calculate the total volume of the body. Fortunately, the most sophisticated methods of child body composition are now feasible without the need to immerse in water. Pletography of aerial displacement is a non-invasive technique that uses the total volume of the body and the mass to derive a model of composition of the body of two components that includes percentage body fat (%BF) and lean body mass (%LBM). This technology has recently been applied to neonatal and child composition studies. – Because an important goal of prenatal assessment is to identify fetuses with abnormal intrauterine growth, airborne pletismography can provide an important insight into which fetal growth parameters more closely reflect the generalized nutritional status of neonates. This study examines the value of prenatal growth parameters and the birth weight to predict the composition of the neonatal body. METHODS This was a prospective and cross-sectional study of gravitational women within 4 days of childbirth. Women were included in their third trimester of pregnancy. Subjects with congenital abnormalities and poorly visualized fetal limbs are excluded due to technical factors. The menstrual age was calculated in strip on the first day of the last normal menstrual period; this information was confirmed by a first-quarter or early-quarter appointment scanner as described above.– Maternal age, gravidity, menstrual age at the time of scanning, gender, ethnicity and presence of obstetric complications were also documented. All participants wrote consistent information and were registered in protocols approved by the Institutional Review Boards of the William Beaumont Hospital, Wayne State University, and the National Institute for Child Health and Human Development Eunice Kennedy Shriver. All ultrasound studies were performed by a single American Registry of Medical Diagnostic and Certified Diagnostic Sonographers that was also experienced with 3DUS. A two-dimensional ultrasound was used to analyze each fetus once. Standard fetal biometric parameters (biparietal diameter (DIAMETER BPARIETAL (BPD), head circumference (HC), AC, wet diaphysic length (HDL) and femoral diaphysic length were measured prospectively. The fetal weights were calculated using two parameters (AC and FDL) models and three parameters (BPD, AC and FDL) described by Hadlock and coworkers.3DUS was also used to acquire fractional arm volumes (AVol) and fractional thigh (TVol), using ultrasonic mechanical hybrid transducers and curved beams (ABB 4-8P, RT). Fractional extremity volumes were measured out of line using commercially available software (4D View 5.0, GE Healthcare). These soft tissue parameters were derived from 50% of the diaphyseal bone length as described above., Each partial volume was subdivided into five equidistant slices that focused along the fetal arm or thigh. The volume of interest was magnified to fill at least half of the screen. The soft tissue borders were improved by using a color filter (sepia) with additional gamma curve adjustments for brightness and contrast. The fractional extremity volumes were calculated after each of the five slices had been manually traced to the cross-sectional view of the extremity. A pediatric air displacement plettography system (PEA POD®, Life Measurement, Inc., Concord, CA, USA) was used, applying densitometry principles of the entire body, to determine %BF and % fatless mass (%FFM) in all neonates within 48 h of delivery. The reliability and accuracy of this system within the day and between days has been well validated in the newborns. In addition, the quality control measures and the automated nature of this equipment minimize the bias of the operators., After calibration of the standardized system and determination of the weight, the neonate was placed in a chamber to measure the volume of the body based on the displacement of the air. These results were used to calculate density for a two-component body composition model. For the purposes of this study, the %BF results were highlighted because %LBM was simply the mathematical difference between the previous and 100% value. Statistical AnalysisThe standard numerical techniques included descriptive calculation statistics such as mean ± SD, minimum, medium and maximum to evaluate the symmetry of data distribution and the validity of the assumption of normality. Histograms were inspected for all continuous variables (including %BF) to evaluate the normality of data distribution because our regression analysis was based on the main underlying assumption that errors were normally distributed. The Anderson-Darling, Kolmogorov-Smirnov and Shapiro-Wilks tests were used to formally test the normality of data distribution. A dispersion matrix of all continuous variables was compiled, including pair correlations, to evaluate the presence of significant interrelations between the different parameters, including %BF. This evaluation helped determine whether transformations would be needed to line data before applying regression analysis. The correlations between each of these parameters and %BF were evaluated using the determination coefficient (R2). Gradual multiple regression analysis was also used to identify the smallest subset of prenatal growth parameters that could explain the greatest variability in %BF. A phased selection procedure was used and a level of P 0.05 was applied for entry into the model. The maximum selection method of R2 improvement was also used to define the best contribution of a single parameter of each predictor by classification in ascending order of R2 values. P values below a α of 0.05 (type I error probabilities) were considered statistically significant. Statistical analysis was performed using the SAS System for Windows version 9.1.3, Service Pak 2 (SAS, Cary, NC, USA). RESULTS The average maternal age ± SD was 30.5 ± 5.2 years. No subject was excluded on the basis of poorly visualized fetal limbs. In a period of study extending from August 2004 to November 2006 8.9 ± 1.4 weeks of menstrual age were delivered. Birth weights were normally distributed with an average value of 3462 ± 579 g. The racial distribution was 72 whites, nine blacks and six Asians. Most pregnancies were not complicated, but some cases had comorbidities such as preeclampsia (n = 2), diabetes (n = 8) and tobacco exposure (n = 5). The average ± SD %BF was 10.6 ± 4.6%. On the contrary, the average percentage of LPG was 89.5 ± 4.7% for this model of two components of child body composition. The average ± SD values for BPD, HC, AC, HDL, FDL and EFW growth parameters are summarized in . The average values for fractional extremities volumes were 36.4 (interquartile range (IQR), 32.7 – 43.1) mL for AVol and 86.9 (IQR, 71.6 – 107.6) mL for TVol. Table 1 Prenatal parameters obtained by two-dimensional ultrasonography in 87 subjects. Growth parameter ± 3D in diameter (cm)9.5 ± 0.4 Head injury (cm)34.6 ± 1.6 abdominal circumference (cm)36.1 ± 2.8 Bone diaphysic length (cm)6.5 ± 0.3 Femoral diaphysics length (cm)7.5 ± 0.4 High circumference (cm)18.4 ±1.9FW This parameter explained only 46.1% of variability in %BF (). None of the other variables, including birth weight, had the level of statistical significance (Contribution of parameters that explain variance in percentage of neonatal body fat. AC, abdominal circumference; BPD, biparietal diameter; EFW, estimated fetal weight; FDL, femoral diaphysical length. DISCUSSION Despite significant advances in image technology, IUGR's definition remains imprecise because of the use of unclear terminology and the lack of coherent diagnostic criteria. To better understand this problem, in Ultrasound in Obstetrics and Gynaecology, a source of peer-reviewed articles literature was produced in the last 12 years (1995-2007). We identified 108 Original Articles and 11 Case Reports that were electronically catalogued using the term "IUGR" of MeSH. Although articles from 25 countries were submitted, the majority came from the United Kingdom (19.3 per cent), the United States (14.3 per cent), Germany (13.4 per cent), Italy (13.4 per cent) and Sweden (9.0 per cent). The terms "IUGR" or "SGA" were defined varyingly using EFW and AC with or without the Doppler sonography. Diagnostic criteria including the fetal growth parameters of EFW, such as AC and FDL, are typically used to calculate EFW and this result is compared to neonatal population standards to establish the risk of adverse results of pregnancy. Fetal nutritional status is generally considered appropriate when the estimated weight is within the normal range. However, EFW does not have the same prognostic importance as the actual weight of birth, as the first cannot be measured directly before birth. Fetal weight estimation models also show reduced accuracy as a result of cumulative measurement errors. A systematic review of 11 different methods of fetal weight estimation concluded that large random errors are an important obstacle to the safe use of EFW in clinical practice because 95% CIs exceeded 14% of the actual birth weight in reported studies. The birth weight is one of the most important postnatal predictors of the pregnancy outcome and is the main growth parameter that is routinely evaluated in newborns. Body composition analysis also considers individual components that contribute to the total weight of the body. These components include water, fat, protein and minerals. Fat is the most variable component of the neonate and is the most important energy store in the bocy., Dual-energy X-ray absorption studies in the neonates also suggest that body weight is the dominant predictor of fat mass. Humans are unique among mammal species because their fetuses deposit significant amounts of fat and have one of the highest percentages of body fat at birth. Sparks and co-workers used published data for the human fetal weight, water and fat composition to estimate that fat deposition represents more than half of the caloric acreation of the 27th week of gestation to the end, and 90% of the term caloric acretion. Fetal fat deposition seemed to increase linearly to approximately 30 weeks. After this crucial point, the deposition of fetal fat increased exponentially to childbirth. Such changes reflect longitudinal studies of volumes of fractionated members in fetuses with normal growth results., Lapillonne and co-workers have also used dual-energy X-ray absortomy to evaluate the body composition of the USG babies within 48 h of delivery. Significant decreases occur in total body fat, lean mass and bone mineral content in such babies compared to AGA fetuses of the same birth weight. Soft tissue can also be evaluated by prenatal ultrasound. As an example, multivariate statistics have been used to demonstrate that the decrease in the soft tissue mass, as indicated in the fetal thigh circumference, is one of the first manifestations of IUGR. Catalano and colleagues used birth weight and other anthropometric parameters to describe the relationship between the composition of the newborn body and the result of fetal growth within 24 hours of delivery. The percentage body fat was calculated from the thickness of the skin and the weights. Seventeen newborns (9%) were USG (the volume is a fundamental physical property that can be used to develop new fetal body composition models. In this research, the gradual multiple regression showed that TVol made the greatest contribution to the variance observed in %BF (46.1%) for neonates. This result was similar to the actual BW, which explained 44.7% of the BF. The TVol represented an additional 21.3% of the total variation in %BF compared to AC alone. Our observations have important implications for the diagnosis and management of fetuses with growth disorders. First, because the composition of the fetal body cannot be quantified directly before delivery, the volume of the fractional limbs can improve our ability to identify and monitor intrauterine growth anomalies. Second, many researchers have defined IUGR with AC measurements or in combination with Doppler ultrasonography.– If the goal is to detect malnourished fetuses, rationality to use unique parameters such as AC, or even EFW, to detect and monitor fetal growth abnormalities may require critical re-examination. In this study, EFW represented only 28-30% of variance in %BF. Third, Barker's hypothesis links low weight to birth to a higher risk of heart disease, diabetes and hypertension in adults as a result of fetal programming. Sayer and Cooper have examined possible mechanisms for the fetal programming of body composition and musculoskeletal development. The low-weight association at birth and the distribution of altered fat, the reduction of muscle mass and low bone mineral content in adults can be caused by a direct effect on the number of cells, the function of altered stem cells and the restoration of regulatory hormonal axes. This study prospectively examined the fetuses during the third trimester of pregnancy. The correlation of prenatal sonographic parameters, such as EFW, to the weight of the birth and composition of the neonatal body, will require a critical examination in previous gestational ages. Despite contemporary obstetric practice to compare EFW with the actual weight of birth, it has been proposed that the use of weight curves at birth for this purpose cannot optimally detect malnourished fetuses because IUGR is overrepresented in premature newborns. However, since the volume of the fractional extremity includes both the fat mass and the lean mass, a sub-analysis of these separate components can offer a new opportunity to evaluate the composition of the fetal body. This task could be improved if automated segmentation of images of the relevant limits of soft tissue is successfully developed for this purpose. As a final note, TVol continues to represent no more than half of the variance in the neonatal percentage. Other new parameters of fetal soft tissues need to be identified and validated to improve our understanding of the development of soft tissue and possibly the subsequent risk of disease in later life. Acknowledgements The authors wish to recognize the technical assistance of Melissa Powell, RDMS and Beverly McNie, BS, CCRP. The research was partially supported by the Perinatological Research Branch, Intramural Research Division, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services.ReferencesFormats: Share , 8600 Rockville Pike, Bethesda MD, 20894 USA
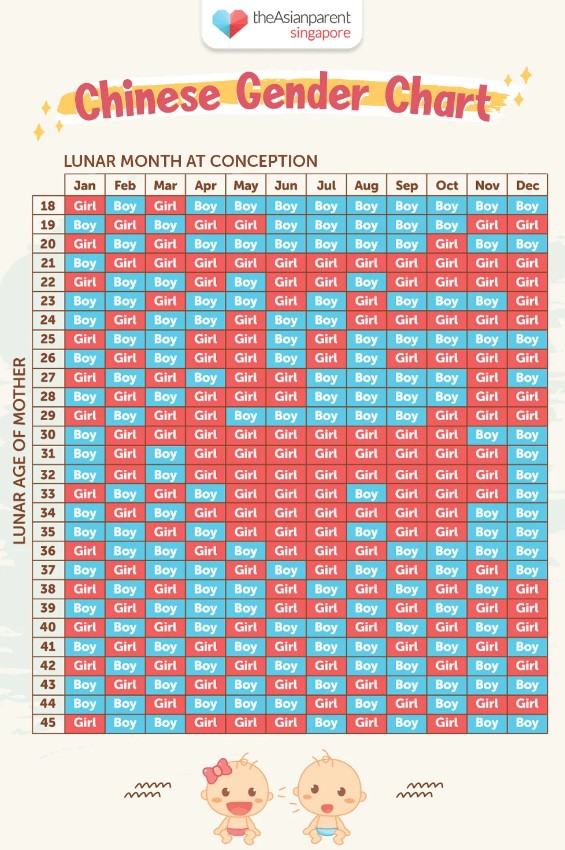
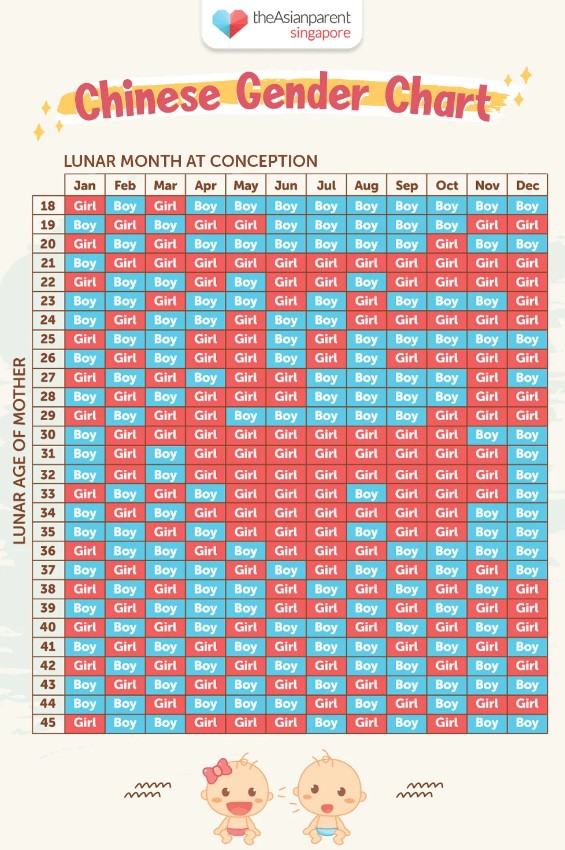
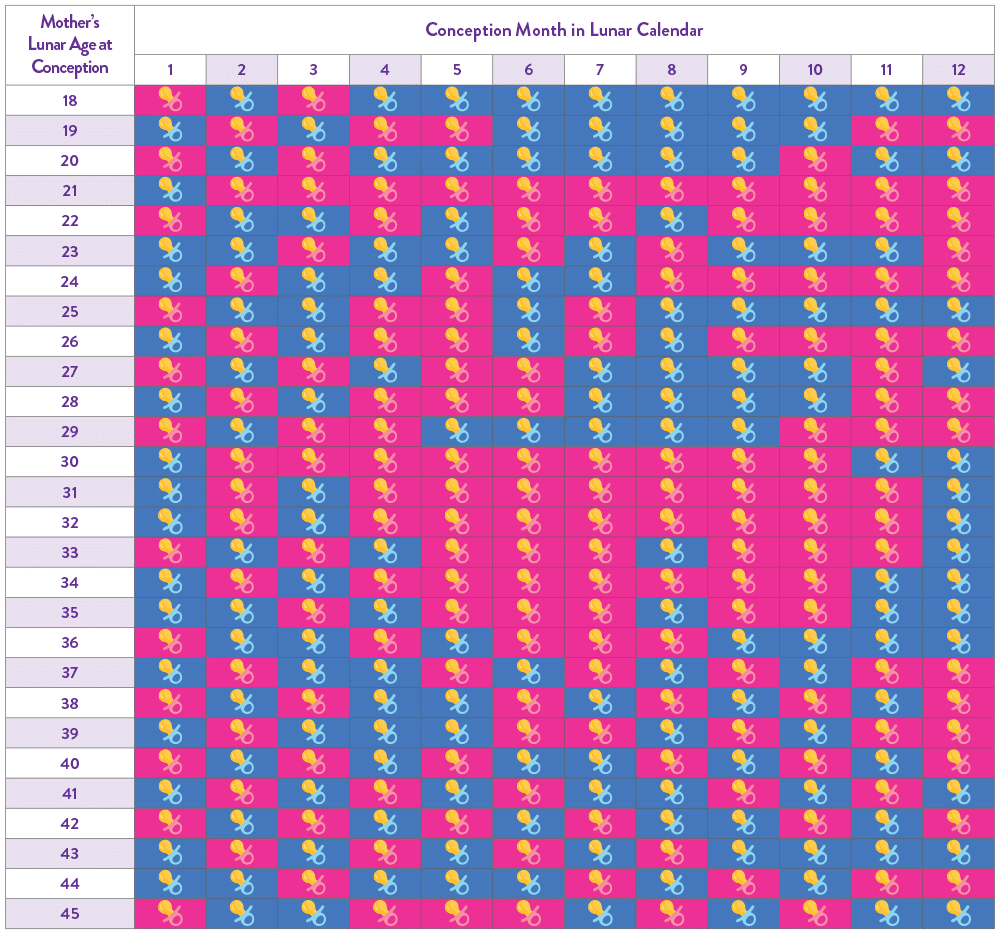
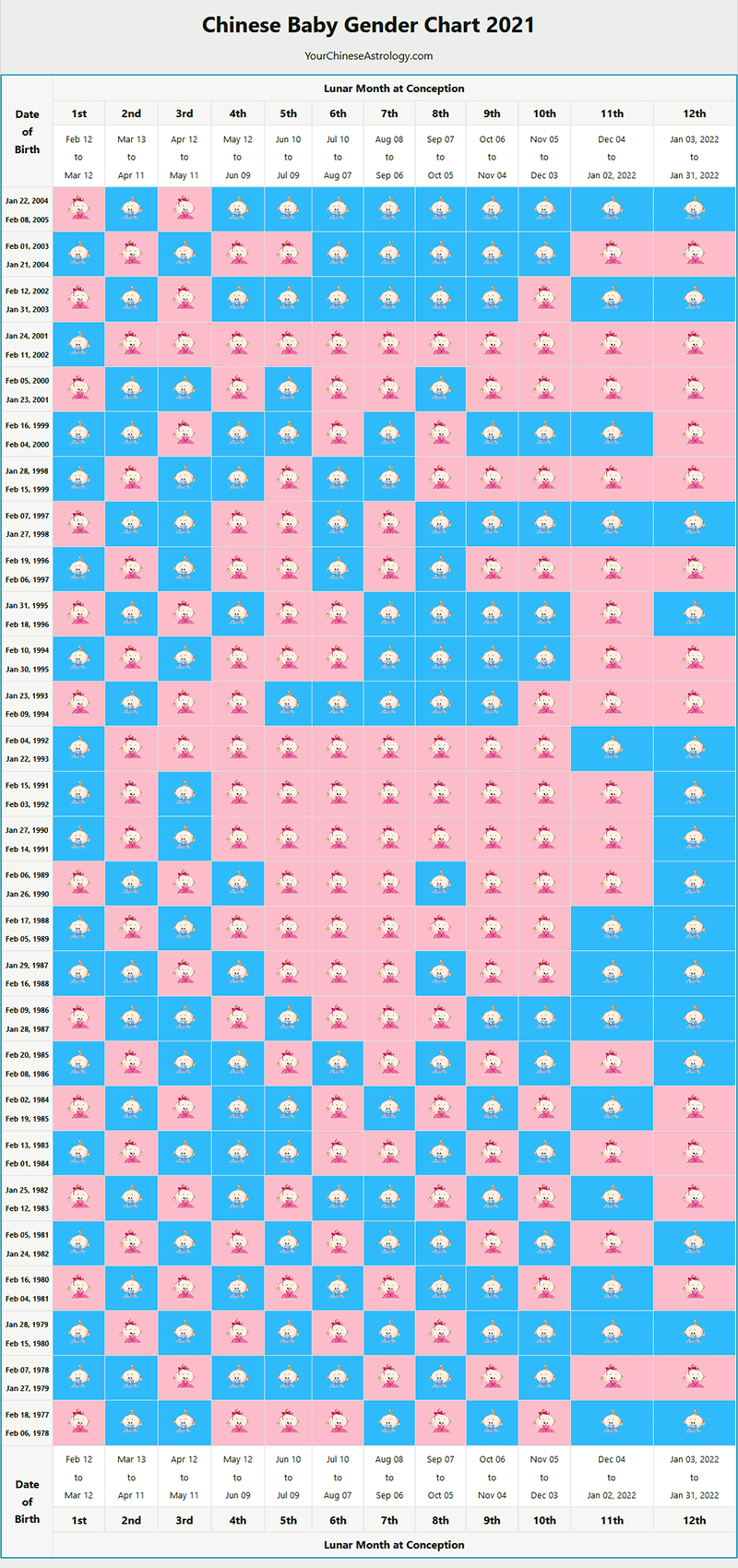
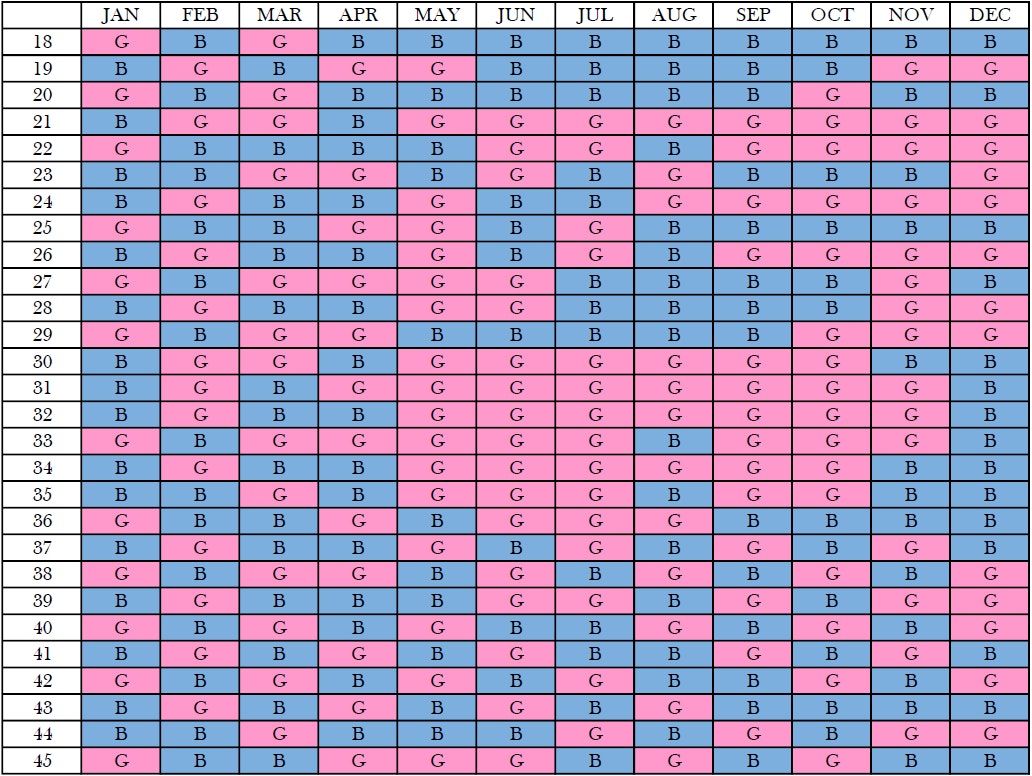
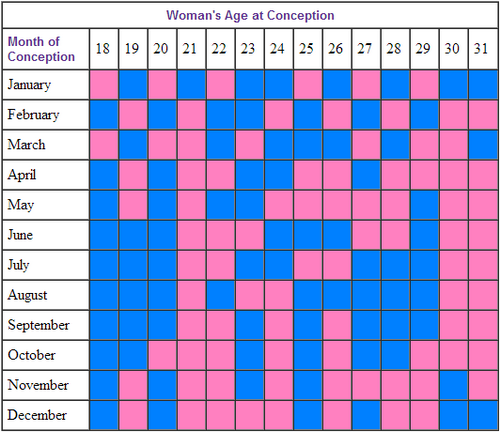
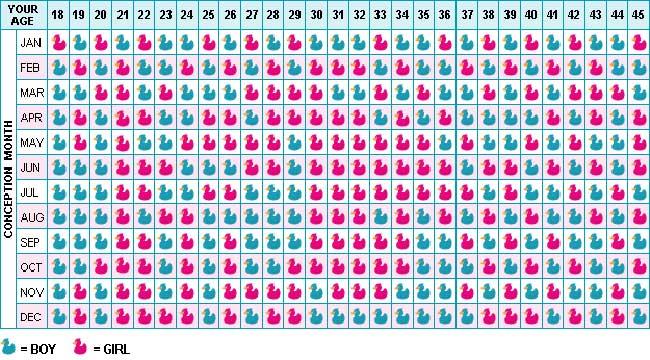
China Pregnancy Calendar China's Gender Chart is an online baby selection and planning tool formulated by the Chinese centuries ago. The Chinese gender prediction chart will help you know how to get pregnant with a child or how to conceive a child. This Chinese gender chart is based on the calculations of the Chinese pregnancy calendar. Knowing when to get pregnant to have a child and what month to become pregnant for a child. Chinese gender chart 2021 Enter the date of birth of the Mother and the year of conception (if it is already conceived) or year of expected conception (if it is a baby) in the form given below. This online gender calendar for Chinese babies will turn age and dates into Chinese year format and perform calculations according to Chinese birth chart. Chinese Gender Calculator for Child Gender Selection Ideally, the Chinese gender chart is used to predict the baby's gender during pregnancy. However, an inverse calculation of the dates will help you step closer to the precise selection of the baby's gender. About the Chinese Letter for Gender PredictionThe Chinese Pregnancy Calendar is an ancient child sex prediction tool. Based on the calculations of this pregnancy schedule, we have created the Chinese Gender Chart. This Chinese baby gender chart is helpful if you are planning to become pregnant and would like to choose your baby's sex before conception. Based on the mother's and conception year, you can predict your baby's gender. Knowing when to conceive for a child in 2022 or what month you need to become pregnant for a child in 2023. Related Links :Pregnancy Yoga, Pregnancy Care Tips with YogaParenting Tips, Articles & Tips Baby Names Pregnancy Weight GainDisclaimer: Although the Chinese gender graph shows a high level of precision, it is not a scientifically proven method to predict the baby's gender.

Pin on baby
How to Conceive a Baby Boy or Girl using Chinese Calendar
How to Conceive a Baby Boy or Girl using Chinese Calendar
Using the Chinese Calendar to Conceive a Boy or a Girl | LoveToKnow
Extraordinary Chinese Calender 2020 For Baby Boy | Chinese calendar gender prediction, Chinese calendar baby gender, Chinese gender calendar
Chinese Birth Chart | Predict Baby Gender Accurately
Try this Chinese Gender Calendar Predictor | Baby Chick
Chinese Gender Predictor, Baby Gender Calendar for Pregnancy
26 Baby boy ideas | gender prediction, gender predictor, gender prediction chart
How to Conceive a Baby Boy or Girl using Chinese Calendar
Chinese Birth Chart | Predict Baby Gender Accurately
Chinese gender prediction chart: can it predict your baby's sex? - MadeForMums
Chinese Calendar For Baby Boy When To Conceive 2019 - ovulation signs
how to conceive a baby boy calendar | Concieving a baby boy, Conceiving a boy, How to conceive
Chinese & Mayan Gender Predictor Calculator And Charts – Scary Mommy
Fertility & Period Tracker on the App Store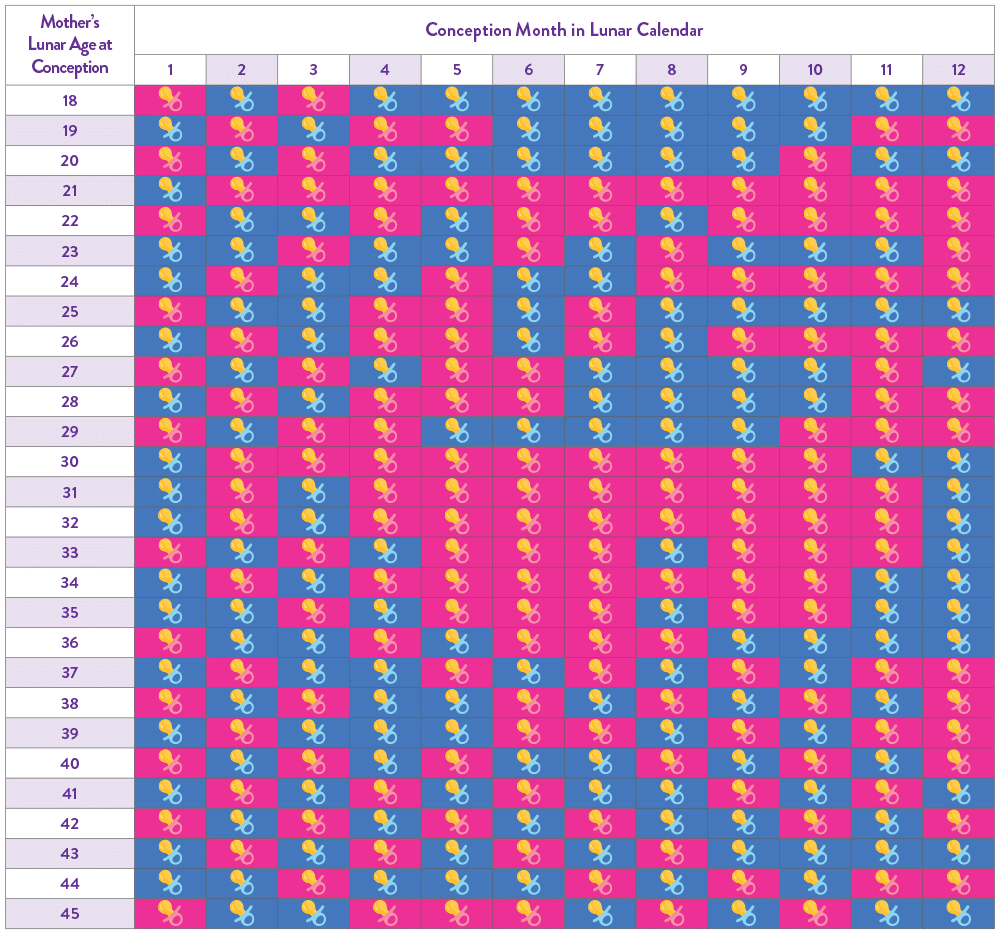
Chinese Calendar Gender Prediction | SneakPeek®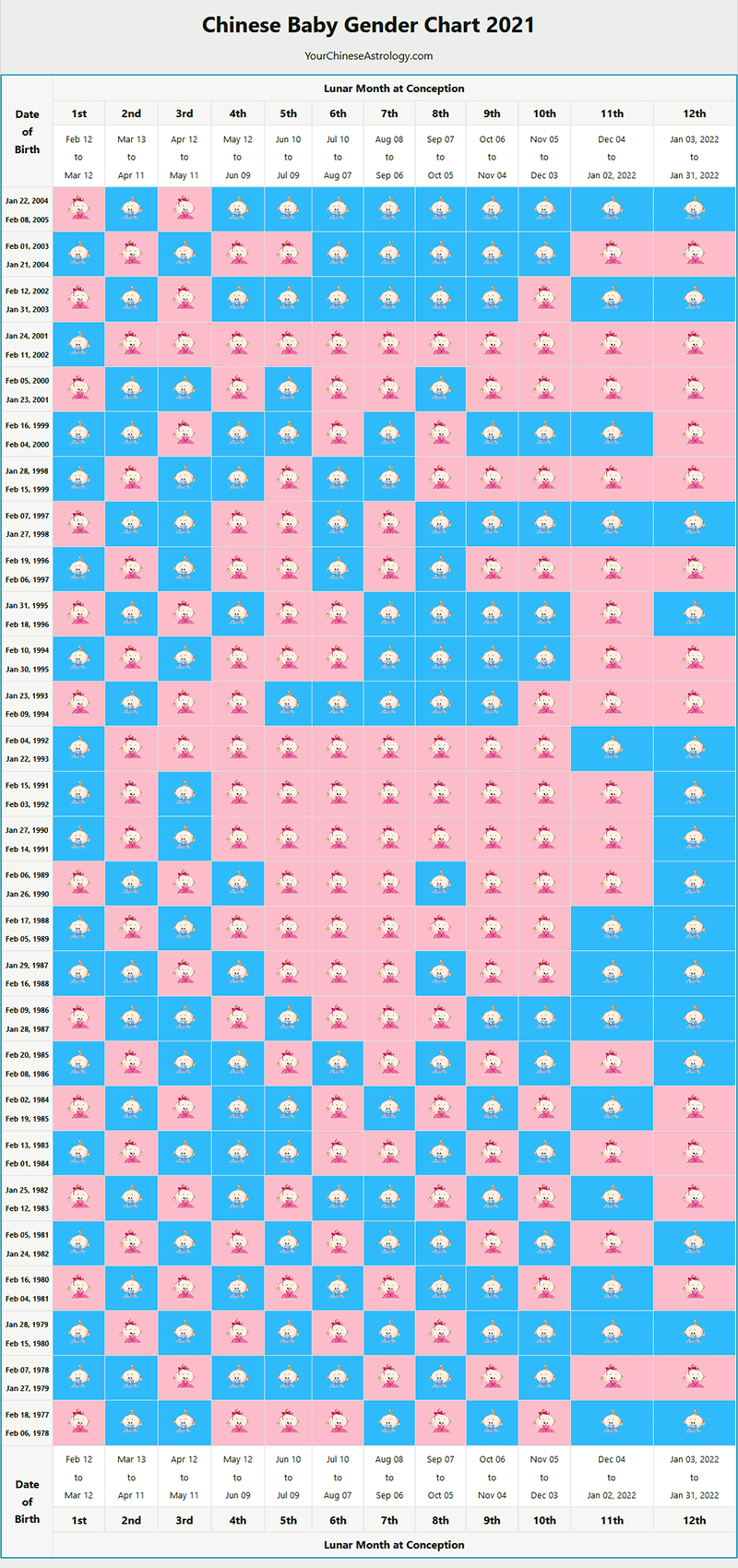
Chinese Gender Calendar, 2021 Baby Gender Prediction Chart, Calculator
chinese baby gender calendar for a baby boy - Gender Picking for your baby
Pin on *kiddy things*
Boy or Girl? 'Predict' Your Baby's Gender With This Chinese Pregnancy Calendar
Chinese Baby Gender Predictor Calendar 2020 | Chinese calendar gender prediction, Chinese gender calendar, Gender prediction
Chinese Calendar For Baby Boy When To Conceive 2020 - ovulation signs
Gender Charts & Calculators - Use Accurate Gender Prediction Tools – The Gender Experts
Chinese Gender Predictor Chart and Calendar Tool
Chinese Birth Chart - Ancient Chinese Calendar to Predict Baby Gender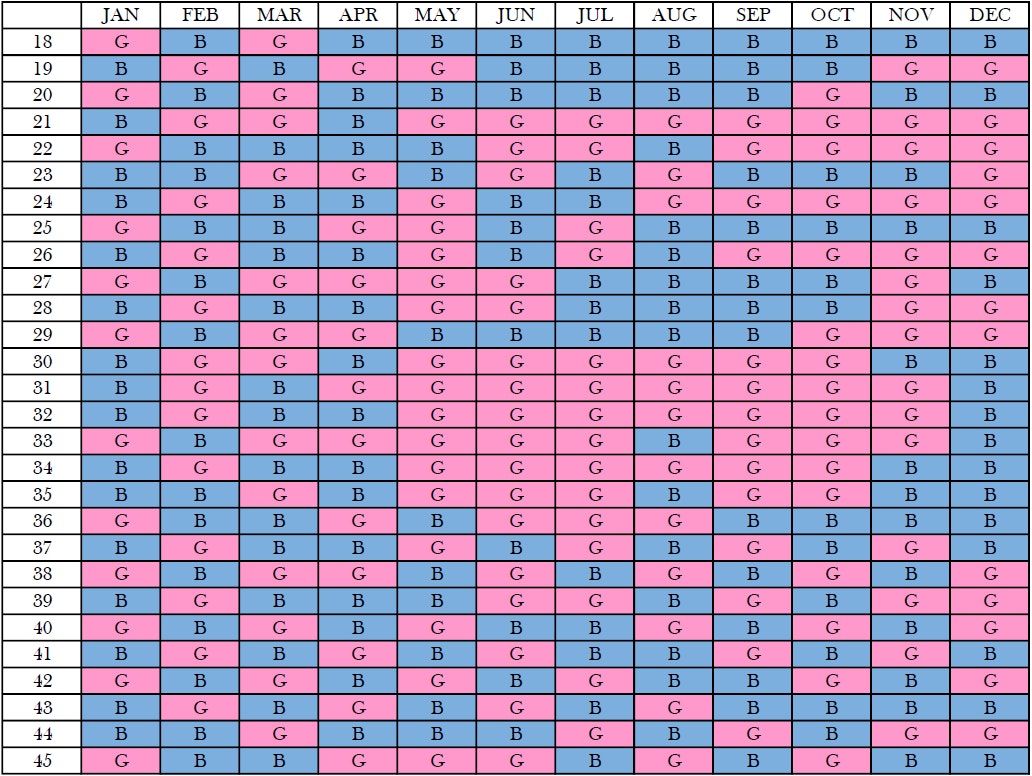
Chinese Gender Predictor Tool and chart | Mother&Baby
3 Ways to Use the Chinese Birth Gender Chart for Gender Selection
How to Conceive a Boy? How to Choose Baby Boy by Chinese Gender Predictor, Gender Calendar Chart
Gender Charts & Calculators - Use Accurate Gender Prediction Tools – The Gender Experts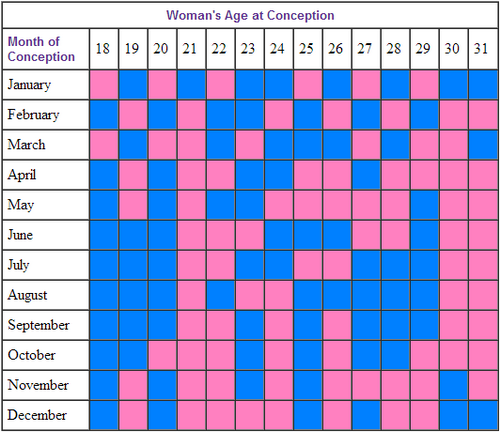
Predict a Baby's Gender by Using the Chinese Gender Calendar | beijingkids online | Beijing | August 16th, 2013 | beijing-kids.com
Baby Gender Prediction: Am I Having a Boy or Girl?? – Happiest Baby
How to get pregnant with a boy ▷ Legit.ng
Pin on Baby Anabelle
Chinese Gender Predictor Chart
Try this Chinese Gender Calendar Predictor | Baby Chick
Chinese Gender Predictor - Chart, Calendar, Test | Gender Calculator
Chinese calendar baby gender 2021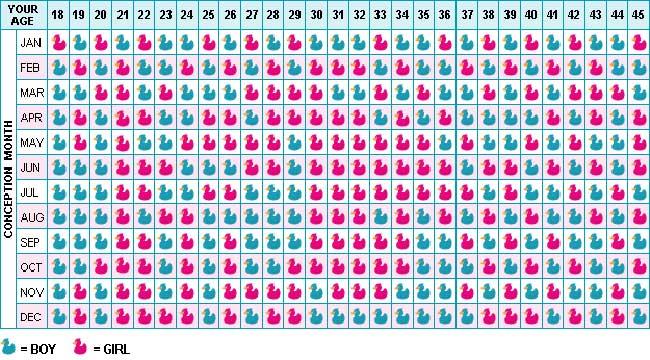
Chinese sex prediction chart | Bounty Parents
 Boy or girl? 'Predict' your baby's gender with this Chinese pregnancy calendar, Lifestyle News - AsiaOne
Boy or girl? 'Predict' your baby's gender with this Chinese pregnancy calendar, Lifestyle News - AsiaOne


























Posting Komentar untuk "when can i conceive a baby boy chinese calendar"